Volume 19, Issue 2 (Mar-Apr 2025)
mljgoums 2025, 19(2): 30-33 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Siahmargoie Z, Hojjati M T, Bazzazi H, Kalavi K, Zakeri M, Joshaghani H. JAK2 mutation, a potential cause of increasing Hemoglobin levels in symptomatic aged women. mljgoums 2025; 19 (2) :30-33
URL: http://mlj.goums.ac.ir/article-1-1743-en.html
URL: http://mlj.goums.ac.ir/article-1-1743-en.html
Zeinab Siahmargoie1 

 , Mohammad Taher Hojjati2
, Mohammad Taher Hojjati2 

 , Hadi Bazzazi3
, Hadi Bazzazi3 

 , Khodaberdi Kalavi3
, Khodaberdi Kalavi3 

 , Mana Zakeri4
, Mana Zakeri4 

 , Hadi Joshaghani3
, Hadi Joshaghani3 




 , Mohammad Taher Hojjati2
, Mohammad Taher Hojjati2 

 , Hadi Bazzazi3
, Hadi Bazzazi3 

 , Khodaberdi Kalavi3
, Khodaberdi Kalavi3 

 , Mana Zakeri4
, Mana Zakeri4 

 , Hadi Joshaghani3
, Hadi Joshaghani3 


1- Iranian Blood Transfusion Organization, Gorgan Branch, Iran
2- Laboratory Sciences Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,mthhematology@gmail.com
3- Laboratory Sciences Research Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Medical Genetics, School of Medicine, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
2- Laboratory Sciences Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,
3- Laboratory Sciences Research Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Medical Genetics, School of Medicine, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
Full-Text [PDF 367 kb]
(255 Downloads)
| Abstract (HTML) (1127 Views)
Results
Out of 72 patients, 24 were women (33.3%) and 48 (66.6%) were men; among them, 39 (54.2%) were negative and 33 (45.5%) were positive for the JAK2 mutation. The data also showed that 15 out of 24 female patients (62.5%) had a positive JAK2 mutation, while in the male patients, 18 out of 48 (37.5%) had the mutation present (p=0.013).
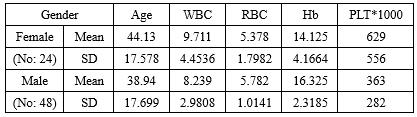
Table 2 shows the information of the patient population by gender without considering the incidence of JAK-2 mutation. The results indicated that there was no significant difference between men and women in any of the investigated parameters. However, the comparison of these parameters without considering the gender and only based on the occurrence of JAK-2 mutation showed that only in the age parameter, there was a significant difference between the two groups; men and women, and with increasing age, the incidence of this disease increases (p=0.024) (Table 3)
Investigations based on the occurrence of JAK2 mutation in the female population also showed that the age parameter in positive and negative groups for the mutation had been significant (p=0.029), so that the age of the negative group was 28.13 ± 13.7 and in positive group it was 53.8 ± 11.8, and in other parameters in female group was not significant (Table 4). However, in the male population, the age of JAK2 positive patients was higher than Negative patients, but there was no significant difference in age and other factors (Table 4). Also, the comparison of all parameters in JAK2 positive mutation patients showed that there was no significant difference in the studied parameters in men and women (Table 5).
Discussion
The influence of gender on the occurrence of PV has been widely discussed in the literature, though findings remain contradictory. Our study revealed a higher prevalence of PV in women (62.5%) compared to men (37.5%), aligning with reports by Godferi et al. (2013) (9) and Payzin (2014) (10). However, conflicting data exist; for instance, Hamid et al. observed a higher mutation rate in men, with a statistically significant correlation between JAK2 V617F and male gender (11). Conversely, Deadmond et al. reported that PV risk was consistently lower in women across all age groups (12). Some studies further suggest that myeloid disorders are more common in younger females, whereas older males exhibit higher susceptibility (13,14). These discrepancies highlight the need to consider gender-specific differences in genotype-phenotype correlations among JAK2-positive patients, particularly in diagnosis, prognosis, and complication management. Given that gender may influence clonal expansion and JAK2 allele burden variability, future research should explore factors driving mitotic recombination events.
The mean age of JAK2-positive cases in our cohort was 45 years for men and 53 years for women, reinforcing the role of age in PV manifestation, as noted in prior studies (11,15). Notably, women with PV exhibited age-dependent susceptibility, with older patients and elevated hemoglobin (Hb) levels being more prone to the disease (Mean age: 53.8 vs. 28 years in unaffected women). In contrast, male patients presented across a broader age range, suggesting divergent pathogenic mechanisms.
Hematological parameters-including WBC, RBC, Hb, and platelet counts-were significantly elevated in JAK2-positive patients, correlating strongly with the mutation. These findings align with Gulbay et al. (16), who reported marked differences in WBC, Hb, HCT, RDW, and PLT between JAK2 V617F-positive and negative individuals.
Conclusion
Our findings suggest that women with Hb levels above the normal range may be at higher risk for PV, underscoring the importance of early screening in this demographic. Additionally, younger men with elevated Hb should also be monitored for PV. These insights could enhance diagnostic accuracy and prognostic stratification in clinical practice.
Acknowledgement
We extend our sincere gratitude to the management and staff of Kavosh Medical Laboratory (Gorgan) for their invaluable support. This work is derived from a Master’s thesis in Biochemistry completed at Islamic Azad University, Gorgan Branch, and reflects the academic research conducted during the author’s graduate training.
Funding sources
The author(s) received no specific funding for this work.
Ethical statement
This study was conducted following the approval of the ethics code (RI.IAU.CHALUS.REC.1401.009) by the Ethics Committee of Islamic Azad University, Chalus branch.
Conflicts of interest
The Authors had no Conflicts of interest
Author contributions
Zeinab Siahmargoie Performing the test; Mohammad Taher Hojjati Supervision, Final validation of the article; Hadi Bazzazi Writing draft of the article and Data analysis; Khodaberdi Kalavi, Data interpretation and technical consultant; Mana Zakeri Writing draft of the article and Statistical analysis; Hadi Joshaghani Clinical consultant and Writing draft of the article.
Data availability statement
All data produced or analyzed during this study are contained within this published article.
Full-Text: (27 Views)
Introduction
Erythrocytosis, defined as an elevated red blood cell (RBC) count, is classified into relative erythrocytosis (Caused by reduced plasma volume/hemoconcentration) or absolute erythrocytosis (Characterized by increased RBC mass) (1). Absolute erythrocytosis may arise from a clonal bone marrow disorder, such as Polycythemia Vera (PV), which has an incidence of 0.84%, or secondary causes (e.g., physiologic or pathologic factors), with a prevalence of 6%-8% (2).
PV is a chronic myeloproliferative neoplasm (MPN) marked by clonal expansion of myeloid lineage cells, predominantly erythrocytes, necessitating differentiation from other MPNs (3). Diagnostic criteria for PV have evolved: the 2008 World Health Organization (WHO) guidelines used hemoglobin (Hb) thresholds of >18.5 g/dL (Men) and >16.5 g/dL (Women) as surrogates for elevated RBC mass (4). The 2016 revision lowered these thresholds to >16.5 g/dL (Men) and >16 g/dL (Women), with additional hematocrit cutoffs (>49% for men, > 48% for women) (5).
A pivotal advancement in PV understanding came in 2005 with the discovery of the somatic JAK2 V617F mutation. The JAK2 gene, located on 9p24, encodes a non-receptor tyrosine kinase critical for the JAK-STAT signaling pathway. This pathway regulates erythropoiesis, influencing proliferation, differentiation, and apoptosis of erythroid progenitors (6,7). The V617F mutation causes constitutive JAK2 activation, leading to erythropoietin (EPO)-independent erythroid growth, uncontrolled proliferation, and subsequent Hb elevation (8).
In this study, we investigated the prevalence of JAK2 mutations in individuals with age- and gender-adjusted elevated Hb levels, referred to our laboratory for clinical evaluation.
Methods
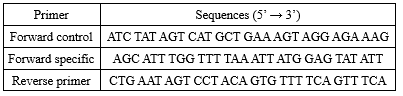
This descriptive cross-sectional study investigated JAK2 mutations in 60 patients exhibiting elevated hemoglobin levels according to WHO criteria (5), with an initial clinical suspicion of polycythemia vera (PV). The patients, referred by oncologists for laboratory analysis, were enrolled after approval by Islamic Azad University, Gorgan Branch (Registration code: 162474677). Approximately 4 mL of whole blood was collected in EDTA tubes from each participant, and a complete blood count (CBC) was performed using an automated Sysmex KX-21N analyzer (Sysmex, Japan) to assess key hematological parameters, including white blood cell (WBC) count, platelet (PLT) count, Hb level, and hematocrit (Hct). Demographic data were recorded for all patients, and written informed consent was obtained before inclusion in the study. Genomic DNA was extracted from the samples using the AccuPrep® Genomic DNA Extraction Kit (Bioneer, Korea) following the manufacturer’s instructions, and the purified DNA was stored at 4°C until further analysis. To detect the JAK2 V617F mutation, allele-specific oligonucleotide polymerase chain reaction (ASO-PCR) was performed using a reaction mixture containing 20–200 ng of template DNA, 20 μM master mix, 5 μM forward control primer (FC), 5 μM forward-specific primer (FS), 5 μM reverse primer, 5 U/μL Taq DNA polymerase, and nuclease-free distilled water. The primer sequences and PCR amplification conditions are provided in Tables 1 and 2, respectively.
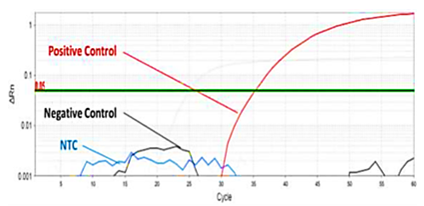
The amplification conditions include initial denaturation at 95°C for 10 min, followed by 14 cycles of denaturation (94°C for 20 sec), annealing (65°C, 60 sec), and extension (72°C for 60 sec). These cycles were followed by a final extension step at 72°C for 5 min. The results were analyzed by Lightcycler96 (Roche, Germany) (Figure 1).
Erythrocytosis, defined as an elevated red blood cell (RBC) count, is classified into relative erythrocytosis (Caused by reduced plasma volume/hemoconcentration) or absolute erythrocytosis (Characterized by increased RBC mass) (1). Absolute erythrocytosis may arise from a clonal bone marrow disorder, such as Polycythemia Vera (PV), which has an incidence of 0.84%, or secondary causes (e.g., physiologic or pathologic factors), with a prevalence of 6%-8% (2).
PV is a chronic myeloproliferative neoplasm (MPN) marked by clonal expansion of myeloid lineage cells, predominantly erythrocytes, necessitating differentiation from other MPNs (3). Diagnostic criteria for PV have evolved: the 2008 World Health Organization (WHO) guidelines used hemoglobin (Hb) thresholds of >18.5 g/dL (Men) and >16.5 g/dL (Women) as surrogates for elevated RBC mass (4). The 2016 revision lowered these thresholds to >16.5 g/dL (Men) and >16 g/dL (Women), with additional hematocrit cutoffs (>49% for men, > 48% for women) (5).
A pivotal advancement in PV understanding came in 2005 with the discovery of the somatic JAK2 V617F mutation. The JAK2 gene, located on 9p24, encodes a non-receptor tyrosine kinase critical for the JAK-STAT signaling pathway. This pathway regulates erythropoiesis, influencing proliferation, differentiation, and apoptosis of erythroid progenitors (6,7). The V617F mutation causes constitutive JAK2 activation, leading to erythropoietin (EPO)-independent erythroid growth, uncontrolled proliferation, and subsequent Hb elevation (8).
In this study, we investigated the prevalence of JAK2 mutations in individuals with age- and gender-adjusted elevated Hb levels, referred to our laboratory for clinical evaluation.
Methods
This descriptive cross-sectional study investigated JAK2 mutations in 60 patients exhibiting elevated hemoglobin levels according to WHO criteria (5), with an initial clinical suspicion of polycythemia vera (PV). The patients, referred by oncologists for laboratory analysis, were enrolled after approval by Islamic Azad University, Gorgan Branch (Registration code: 162474677). Approximately 4 mL of whole blood was collected in EDTA tubes from each participant, and a complete blood count (CBC) was performed using an automated Sysmex KX-21N analyzer (Sysmex, Japan) to assess key hematological parameters, including white blood cell (WBC) count, platelet (PLT) count, Hb level, and hematocrit (Hct). Demographic data were recorded for all patients, and written informed consent was obtained before inclusion in the study. Genomic DNA was extracted from the samples using the AccuPrep® Genomic DNA Extraction Kit (Bioneer, Korea) following the manufacturer’s instructions, and the purified DNA was stored at 4°C until further analysis. To detect the JAK2 V617F mutation, allele-specific oligonucleotide polymerase chain reaction (ASO-PCR) was performed using a reaction mixture containing 20–200 ng of template DNA, 20 μM master mix, 5 μM forward control primer (FC), 5 μM forward-specific primer (FS), 5 μM reverse primer, 5 U/μL Taq DNA polymerase, and nuclease-free distilled water. The primer sequences and PCR amplification conditions are provided in Tables 1 and 2, respectively.
The amplification conditions include initial denaturation at 95°C for 10 min, followed by 14 cycles of denaturation (94°C for 20 sec), annealing (65°C, 60 sec), and extension (72°C for 60 sec). These cycles were followed by a final extension step at 72°C for 5 min. The results were analyzed by Lightcycler96 (Roche, Germany) (Figure 1).
|
Table 1. Allele-specific oligonucleotide-polymerase chain reaction primers
 |
Results
Out of 72 patients, 24 were women (33.3%) and 48 (66.6%) were men; among them, 39 (54.2%) were negative and 33 (45.5%) were positive for the JAK2 mutation. The data also showed that 15 out of 24 female patients (62.5%) had a positive JAK2 mutation, while in the male patients, 18 out of 48 (37.5%) had the mutation present (p=0.013).
Table 2 shows the information of the patient population by gender without considering the incidence of JAK-2 mutation. The results indicated that there was no significant difference between men and women in any of the investigated parameters. However, the comparison of these parameters without considering the gender and only based on the occurrence of JAK-2 mutation showed that only in the age parameter, there was a significant difference between the two groups; men and women, and with increasing age, the incidence of this disease increases (p=0.024) (Table 3)
Investigations based on the occurrence of JAK2 mutation in the female population also showed that the age parameter in positive and negative groups for the mutation had been significant (p=0.029), so that the age of the negative group was 28.13 ± 13.7 and in positive group it was 53.8 ± 11.8, and in other parameters in female group was not significant (Table 4). However, in the male population, the age of JAK2 positive patients was higher than Negative patients, but there was no significant difference in age and other factors (Table 4). Also, the comparison of all parameters in JAK2 positive mutation patients showed that there was no significant difference in the studied parameters in men and women (Table 5).
|
Table 3. Comparison of these parameters without gender discrimination based on the occurrence of the JAK2 mutation
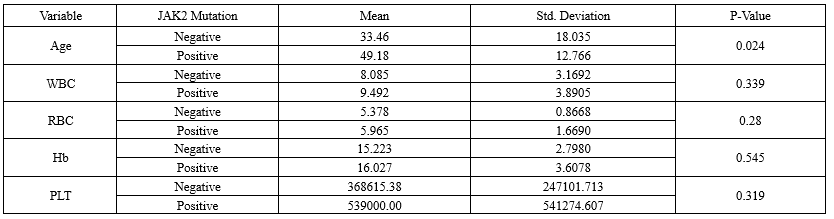 Table 4. Comparison of parameters of patients by gender based on the presence or absence of mutation 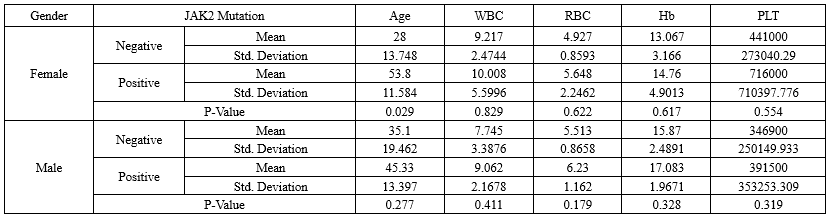 Table 5. Comparison of blood parameters of JAK2-positive patients according to gender 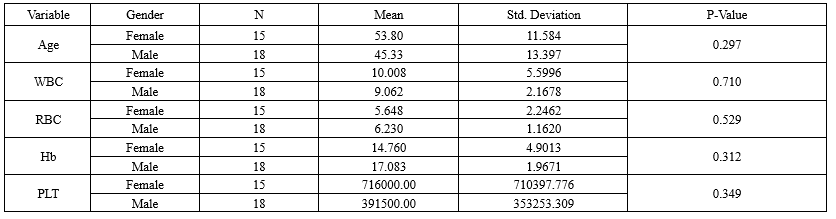 |
Discussion
The influence of gender on the occurrence of PV has been widely discussed in the literature, though findings remain contradictory. Our study revealed a higher prevalence of PV in women (62.5%) compared to men (37.5%), aligning with reports by Godferi et al. (2013) (9) and Payzin (2014) (10). However, conflicting data exist; for instance, Hamid et al. observed a higher mutation rate in men, with a statistically significant correlation between JAK2 V617F and male gender (11). Conversely, Deadmond et al. reported that PV risk was consistently lower in women across all age groups (12). Some studies further suggest that myeloid disorders are more common in younger females, whereas older males exhibit higher susceptibility (13,14). These discrepancies highlight the need to consider gender-specific differences in genotype-phenotype correlations among JAK2-positive patients, particularly in diagnosis, prognosis, and complication management. Given that gender may influence clonal expansion and JAK2 allele burden variability, future research should explore factors driving mitotic recombination events.
The mean age of JAK2-positive cases in our cohort was 45 years for men and 53 years for women, reinforcing the role of age in PV manifestation, as noted in prior studies (11,15). Notably, women with PV exhibited age-dependent susceptibility, with older patients and elevated hemoglobin (Hb) levels being more prone to the disease (Mean age: 53.8 vs. 28 years in unaffected women). In contrast, male patients presented across a broader age range, suggesting divergent pathogenic mechanisms.
Hematological parameters-including WBC, RBC, Hb, and platelet counts-were significantly elevated in JAK2-positive patients, correlating strongly with the mutation. These findings align with Gulbay et al. (16), who reported marked differences in WBC, Hb, HCT, RDW, and PLT between JAK2 V617F-positive and negative individuals.
Conclusion
Our findings suggest that women with Hb levels above the normal range may be at higher risk for PV, underscoring the importance of early screening in this demographic. Additionally, younger men with elevated Hb should also be monitored for PV. These insights could enhance diagnostic accuracy and prognostic stratification in clinical practice.
Acknowledgement
We extend our sincere gratitude to the management and staff of Kavosh Medical Laboratory (Gorgan) for their invaluable support. This work is derived from a Master’s thesis in Biochemistry completed at Islamic Azad University, Gorgan Branch, and reflects the academic research conducted during the author’s graduate training.
Funding sources
The author(s) received no specific funding for this work.
Ethical statement
This study was conducted following the approval of the ethics code (RI.IAU.CHALUS.REC.1401.009) by the Ethics Committee of Islamic Azad University, Chalus branch.
Conflicts of interest
The Authors had no Conflicts of interest
Author contributions
Zeinab Siahmargoie Performing the test; Mohammad Taher Hojjati Supervision, Final validation of the article; Hadi Bazzazi Writing draft of the article and Data analysis; Khodaberdi Kalavi, Data interpretation and technical consultant; Mana Zakeri Writing draft of the article and Statistical analysis; Hadi Joshaghani Clinical consultant and Writing draft of the article.
Data availability statement
All data produced or analyzed during this study are contained within this published article.
Research Article: Research Article |
Subject:
Laboratory hematology
Received: 2023/11/4 | Accepted: 2024/04/6 | Published: 2025/04/14 | ePublished: 2025/04/14
Received: 2023/11/4 | Accepted: 2024/04/6 | Published: 2025/04/14 | ePublished: 2025/04/14
References
1. Tefferi A, Vannucchi AM, Barbui T. Polycythemia vera: 2024 update on diagnosis, risk-stratification, and management. Am J Hematol. 2024;99(4):697-718. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Mithoowani S, Laureano M, Crowther MA, Hillis CM. Investigation and management of erythrocytosis. CMAJ. 2020;192(32):E913-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Aladağ E, Aksu S, Demiroğlu H, Sayınalp N, Göker H, Haznedaroğlu IG, et al. Unclassifiable non-CML classical myeloproliferative diseases with. microcytosis: findings indicating diagnosis of polycythemia vera masked by iron deficiency. Turk J Med Sci. 2019;49(5):1560-3. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Alvarez-Larrán A, Ancochea A, Angona A, Pedro C, García-Pallarols F, Martínez-Avilés L, Bellosillo B, Besses C. Red cell mass measurement in patients with clinically suspected diagnosis of polycythemia vera or essential thrombocythemia. Haematologica. 2012;97(11):1704-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Barbui T, Thiele J, Gisslinger H, Kvasnicka HM, Vannucchi AM, Guglielmelli P, et al. The 2016 WHO classification and diagnostic criteria for myeloproliferative neoplasms: document summary and in-depth discussion. Blood Cancer J. 2018;8(2):15. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365(9464):1054-61. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Hematol, Saeidi K. Myeloproliferative neoplasms: current molecular biology and genetics. Crit Rev Oncol Hematol. 2016:98:375-89. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. James C, Ugo V, Casadevall N, Constantinescu SN, Vainchenker W. A JAK2 mutation in myeloproliferative disorders: Pathogenesis and therapeutic and scientific prospects. Trends Mol Med. 2005;11(12):546-54. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Godfrey AL, Chen E, Pagano F, Ortmann CA, Silber Y, Bellosillo B, et al. JAK2V617F homozygosity arises commonly and recurrently in PV and ET, but PV is characterized by expansion of a dominant homozygous subclone. Blood. 2012;120(13):2704-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Payzin KB, Savasoglu K, Alacacioglu I, Ozdemirkiran F, Mutlu BB, Bener S, et al. JAK2 V617F mutation status of 232 patients diagnosed with chronic myeloproliferative neoplasms. Clin Lymphoma Myeloma Leuk. 2014;14(6):525-33. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Hamid M, Shahbazi Z. Prevalence of JAK2 V617F Mutation in Iranian Patients with Myeloproliferative Neoplasms. Arch Med Lab Sci. 2020;6(1):1-7. [View at Publisher] [DOI] [Google Scholar]
12. Deadmond MA, Smith-Gagen JA. Changing incidence of myeloproliferative neoplasms: trends and subgroup risk profiles in the USA, 1973-2011. J Cancer Res Clin Oncol. 2015;141(12):2131-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. McNally RJ, Rowland D, Roman E, Cartwright RA. Age and sex distributions of hematological malignancies in the U.K. Hematol Oncol. 1997;15(4):173-89. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Cartwright RA, Gurney KA, Moorman AV. Sex ratios and the risks of haematological malignancies. Br J Haematol. 2002;118(4):1071-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Nasseri M, Keyfi F, Rahbarian R, Rajabian M, Abbaszadegan MR. Examining the Frequency of the JAK2 (V617F) Mutation in Patients with Myeloproliferative Diseases in North Eastern Iran and the Effect of Treatment Intervention. Rep Biochem Mol Biol. 2020;9(2):188-92. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Gulbay G, Yesilada E, Erkurt MA, Gozukara Bag H , Kuku I, Kaya E. Evaluation of the JAK2 V617F gene mutation in myeloproliferative neoplasms cases: a one-center study from Eastern Anatolia. Turk J Biochemist. 2019;44(4):492-8. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.